A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
When Your Child Has Alpha Thalassemia
Alpha thalassemia is a blood disorder. It affects the production of a protein in the red blood cells (RBCs). This protein, called hemoglobin, allows RBCs to carry oxygen to all parts of the body. Hemoglobin is made up of smaller parts, including alpha globin and beta globin. When problems with alpha globin lead to less hemoglobin in the blood, the condition is called alpha thalassemia. Alpha thalassemia can cause anemia (not enough healthy hemoglobin in the blood). Your child has been diagnosed with alpha thalassemia. Your child’s healthcare provider can discuss treatment options with you.
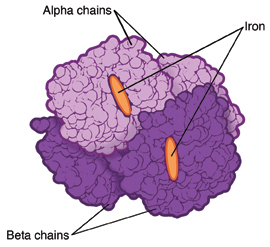 |
| Normal hemoglobin. |
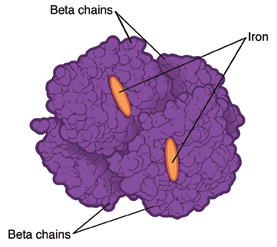 |
| Hemoglobin affected by alpha thalassemia. |
Who is at risk for alpha thalassemia?
This condition affects certain groups more often than others. This includes people who have family members from Southeast Asia, China, India, the Pacific Islands, the Middle East, and the Mediterranean.
What are the types of alpha thalassemia?
Alpha thalassemia is inherited. This means it's passed from parent to child through genes. There are four genes for alpha globin. If any one of these genes is abnormal, the amount of hemoglobin in the body is affected. Alpha thalassemia is broken down into types. The number of problem genes determines the type. The four main types are:
-
Silent carrier state. This type occurs when there is only one abnormal gene. It's unlikely to cause health problems.
-
Alpha thalassemia trait (alpha thalassemia minor). This type occurs when there are two abnormal genes. It may affect the size of the RBCs and cause mild anemia.
-
Hemoglobin H disease. This type occurs when there are three abnormal genes. It's more likely to affect the RBCs and cause moderate to severe anemia. It can also lead to other problems in the body.
-
Alpha thalassemia major. This type occurs when there are four abnormal genes. It's the most severe form of the disease and very rare. Hemoglobin is not able to be produced. A baby with this condition will usually die in the mother’s uterus or soon after birth.
Variations of these types can also occur. Your child’s healthcare provider will tell you about the type your child has. Parents and siblings of a child with alpha thalassemia should be tested for the condition too. A genetic counselor can answer questions you may have.
What are the symptoms of alpha thalassemia?
The symptoms of alpha thalassemia depend on the type. Most silent carriers don't have symptoms. Children with alpha thalassemia trait or hemoglobin H disease may have symptoms that range from mild to severe. These include:
-
Pale skin
-
Crankiness
-
Weakness
-
Tiredness
-
Shortness of breath
-
Trouble doing normal amounts of exercise (exercise intolerance)
-
Fast heartbeat
-
Dizziness or fainting
-
Yellowing of the eyes, skin, or mouth, and dark urine (jaundice)
-
Bone problems including bones of the face or skull being wider
-
Stomach pain and swelling of the belly
-
Not growing as expected
-
Leg ulcers
How is alpha thalassemia diagnosed?
Your healthcare provider may begin testing your child after an abnormal blood count or symptom. Your provider may refer your child to a pediatric hematologist for diagnosis and treatment. This is a doctor who specializes in blood disorders (hematology). The doctor will examine your child and ask about symptoms and health history. Tests will also be done. Most of the tests are performed by taking a blood sample from a vein in the arm or from a finger or heel. Tests may include:
-
Complete blood cell count (CBC). This measures the amounts of types of cells in the blood.
-
Blood smear. This checks the size and shape of blood cells. A drop of blood is looked at with a microscope. A stain is added to make the parts of the blood cells easier to see.
-
Hemoglobin electrophoresis. This is done to check for the amounts and types of hemoglobin in the blood.
-
Other genetic or lab tests. Other tests may be done to evaluate the hemoglobin in the blood.
How is alpha thalassemia treated?
Treatment varies depending on the type of thalassemia your child has and the severity of symptoms.
-
Silent carriers likely need no treatment.
-
Children with alpha thalassemia trait likely need routine checkups and blood count tests.
-
Children with hemoglobin H disease may need treatments that include:
-
Blood transfusions when your child’s blood cell count is too low. Transfusions of RBCs are common. Iron can build up in the blood after frequent transfusions. A treatment called chelation is needed to remove excess iron from the body.
-
Folate supplements to help the body build more RBCs.
-
Surgery to remove the spleen or gallbladder. The spleen is an organ that stores extra blood and helps remove old RBCs from the body. Though done less often, removing the spleen may sometimes be needed. Also, surgery to remove the gallbladder may be needed if gallstones form.
-
Bone marrow transplant. In rare cases, this treatment may be done for children with severe symptoms. Diseased bone marrow cells are replaced with healthy cells from a matched donor. You’ll be told more about this treatment if it is needed.
What are the long-term concerns?
-
Alpha thalassemia is a lifelong condition. Children with moderate to severe forms of anemia need ongoing treatment and supportive care.
-
Parents who both have alpha thalassemia trait can have a child with more severe disease. Talk to a genetic counselor for more information.
Coping with your child's condition
It’s helpful to have support while caring for your child. Think about going for counseling. This can help you and your child deal with any worries or concerns. And seek help from family, friends, community resources, or support groups. Many hospitals also have child life programs, which are designed to help children cope with their condition. A hospital social worker can also answer questions and refer you to other supportive services, if needed. The more you learn about your child’s condition and its treatments, the more in control you may feel.
Online Medical Reviewer:
Adam Levy MD
Online Medical Reviewer:
Dan Brennan MD
Online Medical Reviewer:
Jessica Gotwals RN BSN MPH
Date Last Reviewed:
12/1/2022
© 2000-2026 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.