Peripheral Blood Stem Cell Transplant (PBSCT) for Cancer
Stem cells are immature cells in the bone marrow. They produce all blood cells in the body. They make white blood cells (WBCs), red blood cells (RBCs), and platelets. White cells fight infection. Red cells carry oxygen. Platelets prevent bleeding. Some types of cancer treatments, such as chemotherapy (chemo) and radiation therapy, damage stem cells. This reduces all the cells in the blood. A peripheral blood stem cell transplant (PBSCT) replaces stem cells that are diseased or have been destroyed by cancer treatment. It replaces them with healthy new stem cells from the peripheral blood of the person or a donor.
How PBSC works
Stem cells are collected before cancer treatment. After treatment, the cells are infused into your bloodstream. The cells travel to your bone marrow and begin making new blood cells. There are 2 types of stem cell transplants:
-
Autologous transplant. This uses stem cells that are collected from your own blood and returned to your body.
-
Allogeneic transplant. This uses stem cells from a donor. These stem cells may also be able to kill cancer cells and prevent relapse. This is known as the graft-versus-tumor effect.
The type of transplant used depends on many factors. Both types have advantages and risks.
Autologous PBSCT
This type of transplant comes from your own stem cells.
Before the transplant
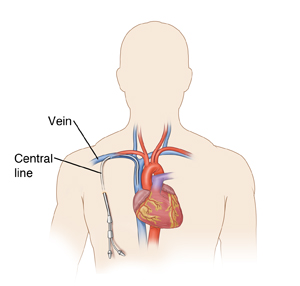
First, the stem cells are removed from your body. This may be done anywhere from 1 month to a few years before your transplant. About 1 week or so before the stem cells are collected, you'll be given medicine to help your bone marrow make more stem cells. Your blood will be tested each day. This is done to see if you have enough stem cells to collect. Before collection, a thin, flexible tube (catheter) is placed in a vein in your neck, chest, or groin. This is called a central line. The collection can take 2 to 4 hours over 1 day or more.
During this time, you'll be connected to a special machine. The machine removes some blood, takes out the stem cells, and returns the blood to you. You may feel a tingling in your lips or hands. The collected stem cells are frozen in a special freezer. Stem cells can be safely stored for many years.
Then, before your transplant, you'll receive conditioning treatment. This consists of high-dose chemo. It may be done with radiation therapy. These procedures are often done in a hospital or outpatient center. They are done a few days before the transplant procedure.
The transplant procedure
The stem cell transplant can be done in a hospital or outpatient center. The stem cells are thawed and then given through your central line into your bloodstream. The procedure can take anywhere from a few hours to a day or more.
You may be given medicines before the stem cell infusion. This is done to prevent reactions to the preservative used when freezing the stem cells. During the transplant, you may also feel short of breath, cough, or have a tight feeling or pain in your chest. You may have high or low blood pressure. A nurse will be with you during the transplant. You'll be watched closely. You'll also get IV (intravenous) fluids. This helps wash out a preservative called DMSO that's used to store the stem cells. DMSO may cause a taste or smell like garlic or creamed corn. You'll notice this during the stem cell transplant and up to 36 hours later.
Allogeneic PBSCT
This type of transplant comes from donor stem cells.
Before the transplant
Like with autologous PBSCT you'll have conditioning treatment before the transplant procedure. The type of treatment you is based on your type of cancer, the type of transplant, and any past treatment. You will receive chemo. This may be high-dose therapy that kills the cells in your bone marrow . Or you may have lower-dose chemo. The type you have depends on certain things. Your provider can tell you which type of conditioning treatment you'll have. You may also receive chemo with radiation therapy. These procedures are often done in a hospital or outpatient center.
The transplant procedure
The stem cells are often transplanted the day after the last dose of chemo. The donor cells are given “fresh.” This means they haven't been frozen and don't contain preservatives. The stem cells are given through your central line into your bloodstream. The procedure can take a few hours. During the transplant, you may also feel short of breath or have a tight feeling in the chest. You may have high or low blood pressure. A nurse will be with you during the transplant. You'll be watched closely. You'll also get IV fluids.
Recovering at Home
Once you return home, follow the instructions you've been given for caring for yourself. These include:
-
Take all medicines as directed. You'll be given medicine to help prevent infection. If you had an allogeneic transplant, you'll take medicine to prevent graft-versus-host disease (GVHD). This is a reaction between the donor stem cells and your body. You may need to take these medicines for up to 1 year.
-
Care for your central line as instructed. Proper care helps prevent serious infection. Don't swim or use hot tubs while you still have your central line.
-
Keep your distance. Stay away from people with colds, the flu, or other contagious illnesses at least until your blood counts have returned to normal. Your immune system may still be immature for up to a year.
-
Stick to low-risk activities. Depending on your type of transplant, you may not be able to do some high-risk activities, such as gardening, for up to 1 year. Discuss this with your healthcare provider.
-
Keep germs at bay. Take care to stay away from germs and molds that may make you sick. Make sure your food is well cooked. Handle food only with clean hands. Don't change litter boxes. Wash your hands often to prevent infection.
When to call your healthcare provider
Call your healthcare provider if you have any of these:
-
Fever of 100.4ºF ( 38ºC) or higher, or as advised by your provider
-
Chest discomfort or pain
-
Trouble breathing
-
Coughing
-
Headache
-
Nausea or vomiting
-
Diarrhea
-
New or worsening skin rash
-
Bruising or bleeding
-
Peeing (urinating) less than normal
-
Irritation, burning feeling, or pain in the rectum
-
Small blisters around the mouth (cold sores) or any part of the body
-
Severe tiredness (fatigue)
-
Any other signs or symptoms indicated by your providers