When Your Child Has Laryngomalacia
Your child has laryngomalacia. This is a condition that causes your child to have noisy breathing. Although the breathing may be loud, your child is not choking. This condition usually goes away over time. Laryngomalacia may range from mild to very serious.
How to say it
lah-RIHNG-goh-mah-LAY-shuh
What is laryngomalacia?
Laryngomalacia happens because the upper part of the voice box (larynx) is floppy or soft. Usually, the epiglottis from the front and two paired pieces of cartilage called the arytenoids from the back are involved in this intermittent closure. The job of the epiglottis is to help keep food from getting into the windpipe (trachea). When your child breathes in (inhales), the floppy epiglottis and arytenoids collapse. This causes your child to have noisy breathing.
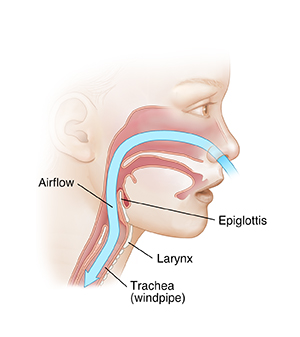 |
| Normal. |
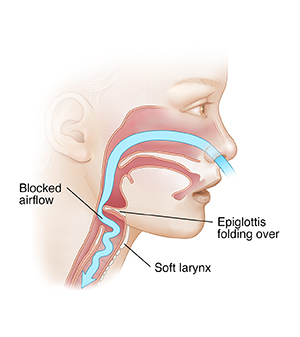 |
| Laryngomalacia. |
What causes laryngomalacia?
It's not known why the condition happens in some children. What is known is that it’s not your fault or the fault of your healthcare provider.
What are the symptoms of laryngomalacia?
Stridor is the high-pitched sound that’s made when your child breathes in. It's the most common symptom of laryngomalacia. Stridor may sound worse when your child is lying on their back or if they have a cold. It may also get worse as your child grows and becomes more active. This is normal. Stridor will stop as the condition goes away.
Gastroesophageal reflux (GER) may develop in children with laryngomalacia. GER occurs when food or stomach acid backs up from the food pipe (esophagus) into the throat or larynx. Stomach contents and acid can irritate and inflame the larynx. This can make the noisy breathing worse. GER usually gets better and goes away with age.
How is laryngomalacia diagnosed?
Your child’s healthcare provider will take a health history and examine your child. The healthcare provider may refer you to an otolaryngologist. This is a healthcare provider who specializes in care of the ears, nose, and throat (ENT). In some cases, your child may need additional tests to confirm the diagnosis and severity. The tests can also rule out other rare causes of stridor. In this case, the provider may order a laryngoscopy. This is a test that lets the provider see inside the larynx. With a laryngoscopy, a thin, usually flexible scope is passed through the nose or mouth into the throat. It allows the ENT healthcare provider to look for problems with the epiglottis, larynx, and the area around the larynx.
How is laryngomalacia treated?
Your child's healthcare provider will closely watch your child. In most cases, the condition goes away without treatment. As your child grows and develops, the epiglottis will likely become stronger and no longer collapse during breathing. In some children with more serious laryngomalacia or who have other defects, surgery may be needed.
If your child has GER along with laryngomalacia, the healthcare provider may prescribe medicine to treat GER.
When to call your child's healthcare provider
Call your child's healthcare provider if your child:
Call 911
Call 911 if your child:
-
Has trouble breathing
-
Turns blue in the face
Tips to reduce reflux
Babies with laryngomalacia may have trouble keeping food down. This means food often comes back up into the mouth (reflux). Follow any instructions the healthcare provider gives you to reduce your child’s reflux. The following precautions for feeding your child can help:
-
Hold your child in an upright position during feeding and at least 30 minutes after feeding. This helps keep food from coming back up.
-
Burp your child gently and often during feeding.
-
Don't give your child juices or foods such as orange juice or oranges that can upset your child’s stomach.
-
Talk with your child’s healthcare provider if food comes up a lot during feeding. You may be told to give your child less milk to prevent reflux.
-
Never lay your baby flat on their back with a propped bottle.
-
Talk with the provider about the correct diet for your child. Some children with reflux may need medicine to help treat GER.