Pyeloplasty
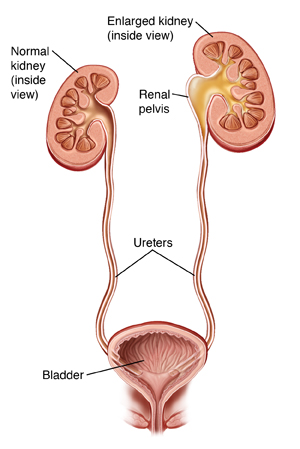
The ureters are the two tubes that carry urine from the kidneys to the bladder. If urine can’t flow freely through a ureter, it builds up in the kidney. This is called ureteropelvic junction (UPJ) obstruction. This may cause symptoms such as bloody urine, pain, fever, and vomiting. It can also cause serious health problems such as infection or kidney damage. People with UPJ obstruction are often born with it, but symptoms may not show up until later in life. Urine flow through the ureter can be blocked by a narrowing (stricture) of the ureter walls. A blood vessel that presses on the ureter can also cause it. Pyeloplasty is surgery to unblock the ureter and let urine flow again.
Getting ready for surgery
Prepare for the surgery as you have been told. In addition:
-
Tell your healthcare provider about all medicines you take. This includes prescription and over-the-counter medicines, vitamins, herbs, and supplements. You may need to stop taking some or all of them before surgery, as instructed by your provider.
-
Don't eat or drink during the 8 hours before your surgery. This includes water, gum, and mints.
-
You may be given a special liquid or medicine to take the day before the surgery. This is to make sure your colon is empty for the surgery.
Two types of surgery
The surgery may be done through several small incisions (laparoscopy). Or it may be done through one larger incision (open surgery). Laparoscopy can't be used in all cases. In some cases, your surgeon may start the procedure with laparoscopy, but for safety reasons must change to open surgery. You and your surgeon will talk about your options.
-
Laparoscopy. The surgeon makes several small incisions in the belly (abdomen). The scope is put through one of the small incisions. The scope sends pictures from inside the abdomen to a video screen. Surgical tools are put through the other incisions. The surgeon may use a method called robotic laparoscopy. The robotic system gives a 3-D view inside the body. It also assists the surgeon’s hand movements.
-
Open surgery. One larger incision is made in the side over the ribs. The surgeon sees and works through this incision. Part of a rib may need to be removed so the surgeon can reach the kidney.
The day of surgery
The surgery takes about 3 to 5 hours. Afterward, you will stay in the hospital for 1 to 3 nights.
Before the surgery begins
-
An IV (intravenous) line is put into a vein in your arm or hand. This line delivers fluids and medicine (such as antibiotics).
-
You may get medicine to prevent blood clots.
-
To keep you free of pain during the surgery, you’re given general anesthesia. This medicine puts you into a deep sleep-like state through the surgery. A tube may be put into your throat to help you breathe.
-
A thin tube (catheter) is placed into your bladder through the urethra. This drains urine during the surgery and for a time afterward.
During the surgery
-
If a part of the ureter is narrowed, that part is cut out. The lower cut end is then sewn to the kidney. Or the ureter and kidney are both cut. Part of the kidney is then used to make the ureter wider. If a blood vessel is pressing on the ureter, it is moved away.
-
A long, flexible tube (stent) is put into the ureter. It reaches from the kidney into the bladder. It's kept in place for 4 to 6 weeks after surgery to help hold the ureter open while it heals.
-
When the surgery is done, all tools are removed. The incisions are closed with stitches, staples, surgical glue, or strips of surgical tape. One or more tubes may be placed near the incisions. These drain fluid from the incision for a short time after surgery.
Recovering in the hospital
After the surgery, you will be taken to the post anesthesia care unit (PACU). You'll be closely monitored as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. When you are awake and stable, you will be taken to your hospital room. While in the hospital:
-
You will be given medicine to manage pain. Let your healthcare providers know if your pain is not controlled.
-
You’ll first receive IV fluids. In a day or so, you will start on a liquid diet. You will then slowly return to a normal diet.
-
As soon as you’re able, you will get up and walk.
-
You’ll be taught coughing and breathing methods to help keep your lungs clear and prevent pneumonia.
-
The catheter in your urethra and any drains will likely be taken out before you leave the hospital. If not, you will be shown how to care for them at home.
Recovering at home
After your hospital stay, you will be released to an adult family member or friend. Have someone stay with you for the next few days to help care for you. Recovery time varies for each person. Your healthcare provider will tell you when you can return to your normal routine. Until then, follow the instructions you have been given. Make sure to:
-
Take all medicines as directed.
-
Follow your healthcare provider’s guidelines for showering. Don't swim, bathe, use a hot tub, or do other activities that will cover the incision with water until your provider says it’s OK.
-
Don't lift anything heavy or do strenuous activities.
-
Don't drive until you are no longer taking prescription pain medicine and your provider says it’s OK.
-
Don't strain during a bowel movement. If needed, take stool softeners as directed by your healthcare provider.
The stent in your ureter will cause the urge to pass urine more often. You may also have some burning and blood in your urine. This is normal and will go away once the stent is removed during a follow-up visit.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Fever of 100.4° F ( 38° C) or higher, or as directed by your provider
-
Symptoms of infection at an incision site, such as increased redness or swelling, warmth, worsening pain, or foul-smelling drainage
-
Bleeding or a large amount of drainage from an incision
-
Blood clots in your urine
-
Leg pain or swelling
-
Inability to urinate
-
Vomiting that doesn’t go away
Call 911
Call 911 right away if you have:
-
Chest pain
-
Trouble breathing
Follow-up care
You will have follow-up visits with your healthcare provider. If sutures or staples need to be removed, this is done 1 to 2 weeks after surgery. The stent in the ureter will be removed in 4 to 6 weeks. About 3 months after surgery, you may have an imaging test. This checks that the ureter is open and the kidney is working normally.
Risks and possible complications
All procedures have some risk. Possible risks of pyeloplasty include:
-
Infection
-
Bleeding (you may need a blood transfusion)
-
Urine leakage at the surgical site
-
Scarring of the ureter
-
Damage to nearby organs
-
Need for further surgery
-
Kidney damage
-
Risks of anesthesia (the anesthesiologist or nurse anesthetist will discuss these with you)